Introduction:
There has been an increase in number of alternative donor [Unrelated donor (UD) or Haploidentical (HIT)] transplants in recent years due to better graft vs. host disease (GVHD) prophylaxis and comparable outcomes with matched sibling transplants. However, viral reactivations frequently complicate these transplants and can lead to organ dysfunction, poor graft function and death. We aimed to analyze incidence, risk factors, and outcomes of viral reactivations in alternative donor transplants at our centre.
Methods:
All UD or HIT transplants performed between January 1st 2009 and February 29th 2020 were included in this retrospective analysis. Conditioning regimen used were either myeloablative (TBI based) or reduced intensity (fludarabine based). All patients received T cell replete grafts. Calcineurin inhibitors (with methotrexate or mycophenolate mofetil) were used for GVHD prophylaxis. Rabbit anti-thymocyte globulin (ATG) was used in UD transplants and post transplant cyclophosphamide was used in HIT.
Cytomegalovirus (CMV) was monitored twice weekly from start of conditioning. Adenovirus (ADV), BK, Epstein Barr virus (EBV) were monitored weekly post engraftment. Monitoring was done by real time quantitative PCR in peripheral blood for CMV, EBV and in blood as well as urine for ADV and BK virus. Parvovirus and Human Herpes virus-6 (HHV-6) were monitored if clinically indicated. Viral reactivation was defined as 2 consecutive readings of >150 copies/mL. Monitoring was stopped after withdrawal of immunosuppressants and restarted with onset of GVHD or use of systemic steroids. Ganciclovir (GCV) was usually preferred for pre-emptive treatment of CMV. Cidofovir (CDV), foscarnet (FOS), artesunate (ART) or leflunomide (LEF) were used when GCV failed or was myelotoxic. Cidofovir was used for ADV disease. Intravenous immunoglobulin (IVIg) prophylaxis was used in all patients.
Primary objective was to estimate the incidence of viral reactivation. Secondary objectives were to explore various risk factors associated with viral reactivations and determine their strength of association using odds ratio (OR).
Results:
Of 334 allogeneic transplants performed during this period, 87 were alternative donor transplants (26 UD and 61 HIT).
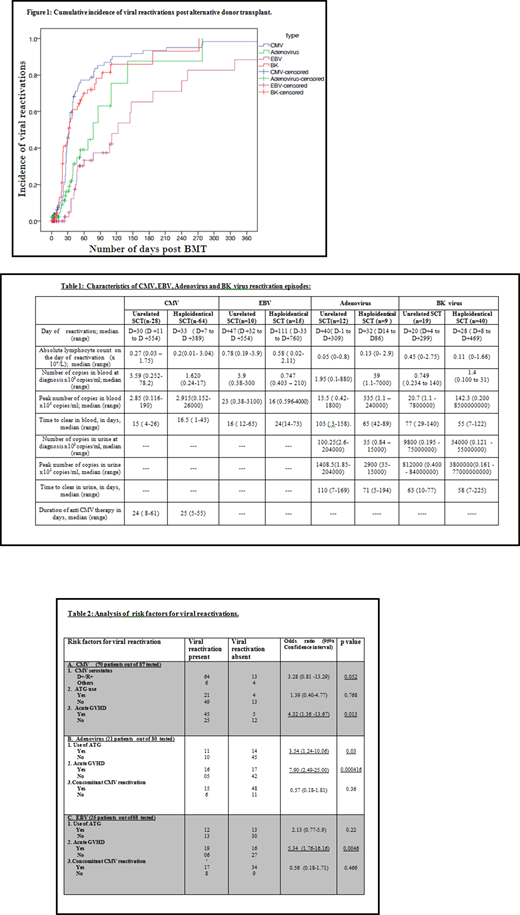
Incidence of CMV reactivation was 80.5 % (92 episodes of CMV reactivations in 70 patients). Two in UD transplant and 4 in HIT developed CMV colitis. Acute GVHD was a significant risk factor for developing CMV reactivation (OR=4.32, 95% CI 1.3-13.6; p=0.013). Pre-emptive 1st line treatment with GCV was used in 59 episodes, ART in 10, LEF in 19, CDV and FOS was used in 1 and 3 episodes each. No deaths were attributed to CMV disease.
Incidence of ADV reactivation was 26% (21 episodes in 80 patients tested). Four patients developed ADV disease and were treated with CDV (ADV colitis in 2, ADV cystitis in 1, and 1 had colitis with CNS involvement) of which 2 died. Use of ATG (OR 3.5, 95% CI 1.2 - 10; p=0.03) and presence of acute GVHD (OR 7.9, 95% CI 2.5- 25; p=0.0004) were significant risk factors of ADV reactivation.
EBV reactivation was seen in 25 of 68 patients tested (incidence 36.7%).Two patients developed post transplant lymphoproliferative disorder requiring therapy with rituximab, of which 1 died.
One out of 15 patients tested by qualitative PCR had HHV 6 reactivation and primary graft failure.
BK viral reactivation was seen in 59 of 71 tested (incidence 83.1%). Grade I and II hemorrhagic cystitis (Droller's grading system) was seen in 12 and 11 patients respectively. Foley's catheterization with bladder irrigation was used in 3 patients and intravesical GCSF was given to 1 patient.
Parvovirus infection was seen in 2 of 12 patients tested, of which 1 was given IVIg.
Cumulative incidence of viral reactivations is shown in Figure 1. Viral reactivation characteristics and risk factors are shown in tables 1 and 2 respectively.
Median OS for the cohort of 87 patients was 52 months. There was no statistically significant impact of viral reactivations on OS.
Conclusion:
Incidence of CMV reactivation is high (80%) in alternative donor HSCT and acute GVHD is a significant risk factor for CMV, ADV and EBV reactivation. Use of ATG is a significant risk factor for ADV reactivation. However, rates of ADV, BK virus, and EBV reactivation requiring intervention were low. Better prophylactic strategies are necessary for prevention of CMV reactivations in alternative donor transplants.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal